
Estate Planning
Advance Directive: How to Create One | GoodTrust
While we typically think of estate planning as only involving things that will happen after your death, advance directives are an essential part of end-of-life planning as well.
Advance directives help your loved ones make major decisions regarding your medical care while you’re still alive, and allow you to communicate your desires if you can't do so on your own. Read on to learn more about:
What an advance directive is
The types of advanced directives
How to determine what to include
How to change your
advance directive
What Is an Advance Directive?
An advance health care directive (sometimes called a medical directive - create yours with GoodTrust here) spells out your medical wishes for end-of-life care. Advance directives are used in life-or-death situations where you're unable to communicate your wishes in the moment or are no longer capable of understanding the gravity of your decisions.
The 1990 Patient Self-Determination Act (PSDA) requires healthcare facilities to ensure patients understand their states' healthcare laws, ask if they have advance directives, and not discriminate based on whether or not someone has an advance directive.
Physicians usually follow advance directives; however, they aren't required to do so in every circumstance. If a request goes against best practices, their facility's policies, or their consciences, they may opt not to follow it.
When this occurs, they're required to tell you or a designated representative the moment they've made this decision. If possible, they should help you transfer to a facility where your medical directive will be honored.
That said, it's typically in the practitioner's best interest to follow your advance directive. Following your wishes provides the healthcare provider with immunity if injury or death occurs because of your directive.
What Is Not Included in Advance Directives?
Your advance directives only involve medical requests. Anything related to your home life (including guardianship of children) or finances is handled through other means.
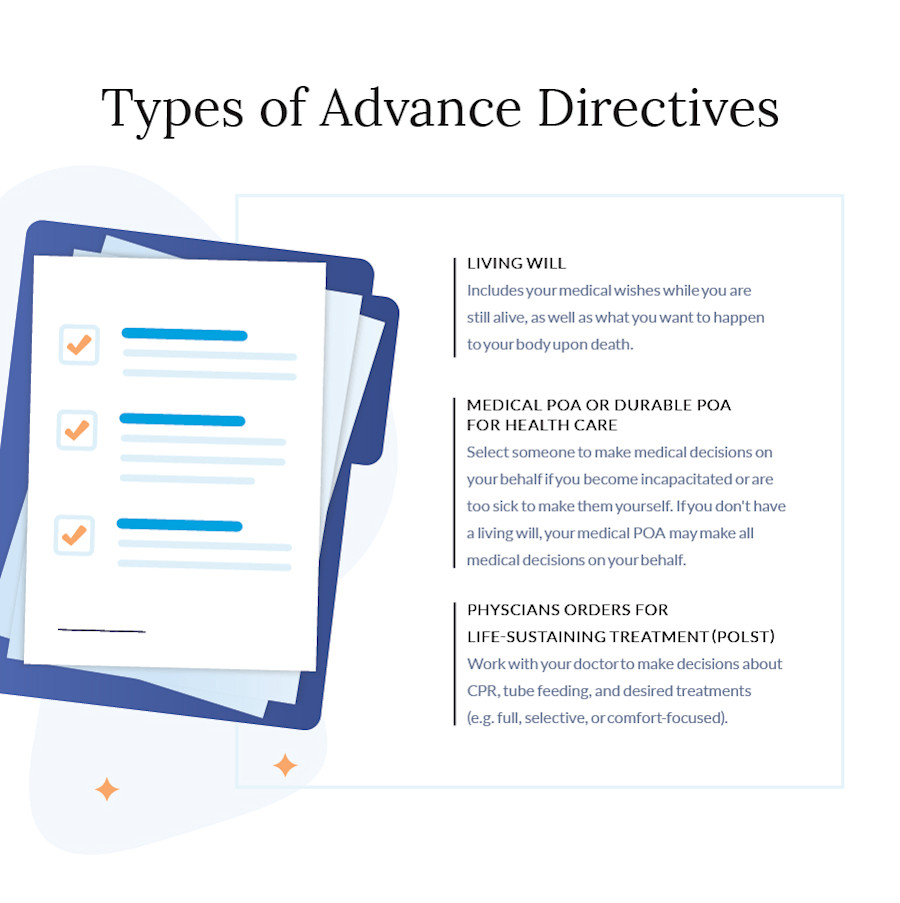
"Advance directive" is a catch-all term for any document detailing what medical care you want if you're unable to communicate your wishes anymore.
There are several types of medical advance directives, including living wills, powers of attorney, and POLSTs.
Living Will
Whether you want every effort made to save your life, live the rest of your days in peace with little intervention, not be resuscitated, or anything in between, you can make your desires known in a living will.
Your living will should also include what you want to happen to your body upon your death. This is especially important if you're an organ donor, as your body should be alive until your team locates recipients.
A living will differs from a last will and testament because it only considers what your medical wishes are while you're still alive. When you create a last will and testament, you declare everything you want to happen with your estate and those in your care upon your death.
Medical POA or Durable POA for Health Care
Power of attorney (POA) allows a person you select to take action and make decisions on your behalf if you're unable to do so.
If you grant someone POA but not durable POA, they're allowed to make decisions for you unless you become incapacitated.
On the other hand, durable POA allows your designated person to make decisions if you can't speak for yourself. As far as advance directives go, you’ll likely grant someone durable POA in case you can’t make healthcare decisions for yourself.
By granting someone durable medical power of attorney (also referred to as durable power of attorney for health care), you’re selecting them to make medical decisions on your behalf if you become incapacitated or are too sick to make them yourself.
If you don't have a living will, your medical POA may make all medical decisions on your behalf.
Physician Orders for Life-Sustaining Treatment (POLST)
Creating your Physician Orders for Life-Sustaining Treatment (POLST) advance directive is a joint effort between you and your medical practitioner. With your doctor's assistance, you make the following decisions:
Decision 1:
Do you want CPR?
Yes: In this case, CPR also includes ventilation, defibrillation, and cardioversion.
No: This is the same as having a DNR (do not resuscitate).
Decision 2:
What are your goals? What treatments do you want?
Full Treatments:
All treatments are allowed, including surgery and intensive care. You may not say "yes" to full treatments and "no" to CPR.
Selective Treatments:
Practitioners may perform life-saving or prolonging treatments, such as IV fluids, antibiotics, and non-invasive airway treatments.
Comfort-Focused Treatments:
Allows for natural death with minimal interventions, which should only provide comfort.
Decision 3:
Do you want tube feeding (medically assisted nutrition)?
Yes, Option 1: Use surgically placed tubes to provide nutrition.
Yes, Option 2: Attempt artificial nutrition without surgical tubes.
No: No attempted artificial nutrition.
Not Discussed or Undecided: Whatever best fits within your previous decisions will occur.
National POLST offers a standardized form you can fill out with your practitioner, though your state may have a preferred version. In most cases, your POLST will be honored in other states.
Once your POLST is complete, your doctor must sign off on it. Ensure your entire medical team has copies.
Keep additional copies in your home, with select loved ones, and for utmost security and accessibility, upload a copy to a digital legacy service.
What to Include in an Advance Directive
When deciding what to include in an advance directive, there are five questions you should ask yourself:
1. Why Do I Want an Advance Directive?
Knowing why you want an advance directive can help you determine what type(s) you need.
There are many reasons to make an advance directive, including:
Wanting to take some stress off of those you love if you become incapacitated
Having a chronic illness that could result in incapacitation
Having a terminal illness
Having strong beliefs about end-of-life issues, especially if they conflict with those of the people around you
Your family may not always get along well, and you want to ensure your wishes are met and alleviate drama
Knowing why you want your advance directive can help you determine which kind(s) you want, who gets durable medical POA, and how explicit you must be in your wishes.
2. Who Do I Want Making Medical Decisions for Me?
When considering potential people to oversee your medical care if you're incapacitated, you need to think about two things:
Who is emotionally capable of carrying out my wishes?
Who will advocate for me with doctors, family members, and others?
When you discuss this topic with your choice for durable medical POA, allow them to say no. It doesn't mean they don't love you; it means they're not the right person for the job.
Consider having a backup listed in case your primary choice is unable to carry out their duties.
3. What Treatments Am I Comfortable With?
Talk through different types of life-saving, life-lengthening, and palliative treatments with your doctor. This can help you made informed decisions when creating your medical directive.
Your beliefs, religious or otherwise, also play a role in your end-of-life care. If you don't have an advance directive, people who don't share, know, or understand your beliefs may make decisions for you.
No matter what influences your decisions, make your advance directive as explicit as possible.
4. What Healthcare Facilities and Practitioners Do I Want Involved?
You can often request your preferred doctor, hospital, or hospice facility. Barring emergencies or situations where your preferred providers can't offer your care, this portion of your directive should be easy to follow.
5. When Do I Want Treatments to Stop?
Many advance directives allow you to determine when you would like all treatments to stop via a quality-of-life statement.
When creating your statement, work with a doctor or lawyer to ensure your wording is precise.
A quality-of-life statement can include:
Your definition of “bad quality of life” – i.e. what symptoms or conditions would you not want life-extending treatment for?
Timing around continued treatment (e.g. End treatment if I have been in a vegetative coma for more than five years.)
Specifics on use of CPR, feeding tubes, and ventilators
Preferences around death. Where and with whom would you like to take your last breaths?
Here’s a sample quality-of-life statement for reference.
How to Create an Advance Directive
"Advance directive" is a catch-all term for all paperwork involving end-of-life care. Here are the basic steps to creating most medical directives:
Make a list of your wishes.
Talk to your choice(s) for durable medical POA. Confirm they are willing to take on the task.
Designate a durable medical POA and spell out your wishes as required by your state. You can find advance directive forms on the for this step.
Create a POLST with your doctor.
Show your complete advance directive to a doctor who can tell you if your requests are reasonable.
Have your advance directives signed as required by your state (may require notarization).
Print off several copies of your advance directive forms, providing them to your medical team and anyone with POA.
Secure your documents by uploading them to your digital legacy account.
Put an in your wallet so practitioners can get a copy.
With GoodTrust, you can create a medical directive online in minutes. Click here if you’re ready to get started.
Make Changes to Your Advance Directives
You can change your advance directive whenever you want. Some common reasons for changing it include:
New diagnosis
Your overall health has declined
Divorce, death of a spouse, or marriage
POA replacement
You're moving to a new state and need to fill out their required paperwork
Ten years have passed (the recommended amount of time between reviews)
There isn't one set of steps for changing your advance directives; rules vary by state and type of directive. However, in all cases, you should:
Ensure the person with medical POA knows you've made changes.
Give copies of the new medical directive to all relevant parties and practitioners.
Upload a new version to your digital legacy platform.
Make sure all copies of the old advance directive are destroyed.
Ensure You Get the Medical Care You Want
Advance directives, also called medical directives, are an integral piece of estate planning.
Whether you choose to use a living will, durable medical POA, POLST, or a combination, having an advance directive can leave you with peace of mind and your loved ones with a plan if you can't make decisions for yourself.
You can help others carry out your wishes by ensuring all your estate planning and other digital afterlife documents are in one easy-to-find place, such as a GoodTrust profile.